How to Navigate Emotional Changes After Weight Loss Surgery: Tips and Support
Emotional changes are a common part of the journey after weight loss surgery. This blog explores how to navigate challenges like anxiety, depression, and body image issues. Discover ways to recognize triggers, develop healthy coping strategies, and build a supportive network to maintain your emotional well-being post-surgery.
Key Takeaways
- Emotional changes post-weight loss surgery are common and can include feelings of anxiety, vulnerability, and depression; recognizing these emotions is crucial for adjustment.
- Developing healthy coping mechanisms, such as mindfulness and engaging in hobbies, can significantly improve emotional well-being and help manage emotional eating.
- Building a strong support system and setting realistic expectations are essential for navigating the emotional journey after weight loss surgery.
Understanding Emotional Changes Post-Surgery
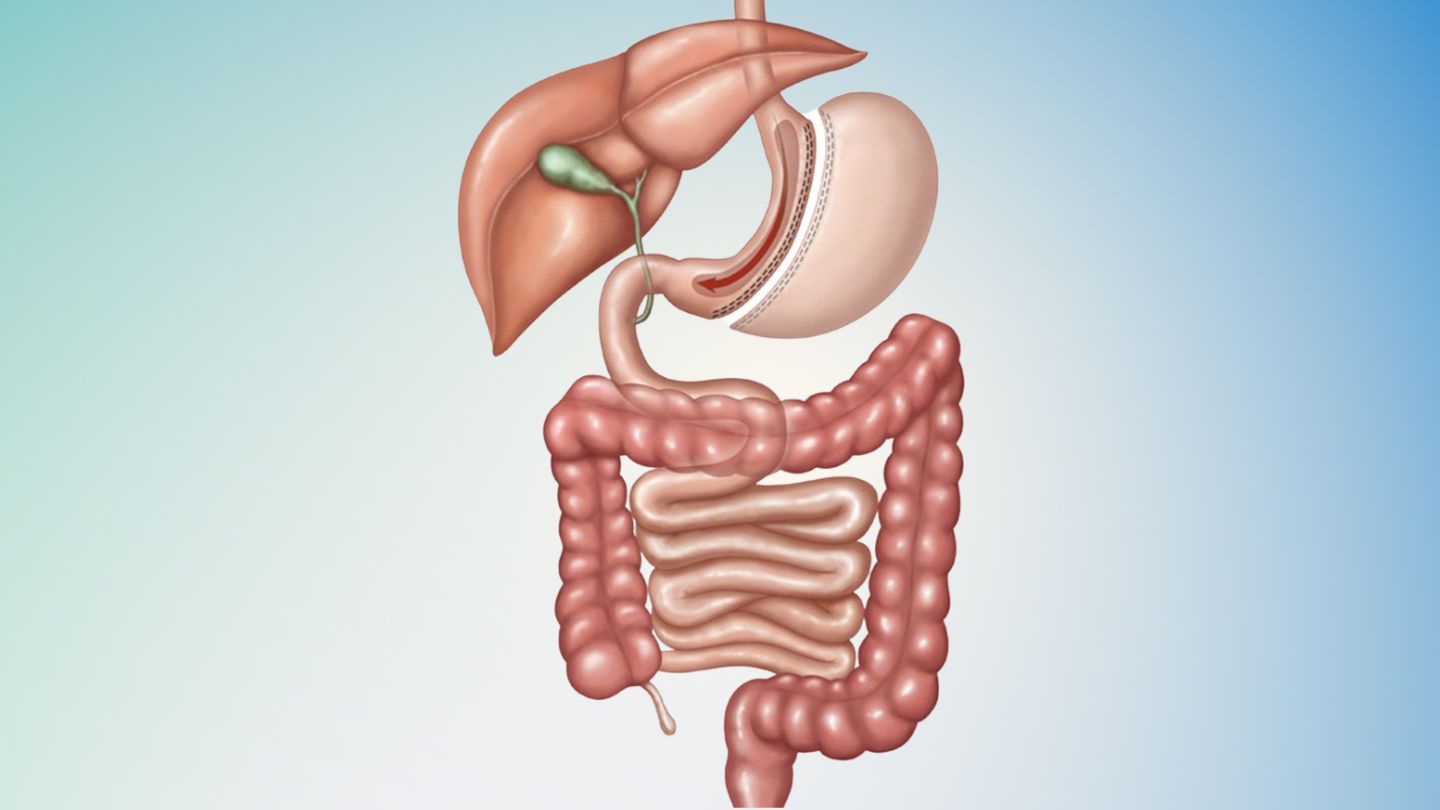
Undergoing weight loss surgery, such as gastric bypass or other forms of bariatric surgery, can result in a wide array of emotions. Patients may oscillate between heightened irritability and depression while adapting to the alterations in their lifestyle. The emotional strain from this type of surgery often originates from the demands of significant lifestyle adjustments like strict dietary regimens or confronting physical side effects, including dumping syndrome.
After undergoing weight loss surgery, it’s not uncommon for patients to grapple with a sense of vulnerability and trepidation toward change. They typically experience a mixture of eagerness and nervousness regarding the procedure, which can be daunting to manage. Mental health issues like anxiety and stress frequently arise as individuals come to terms with their altered way of life, driven by an apprehension towards unfamiliar situations.
Post-surgery emotional adjustments might include battling against tendencies for emotional eating or potentially developing eating disorders such as bulimia or anorexia, along with various psychological concerns.
Nevertheless, there is a positive aspect. Attaining newfound health milestones coupled with self-acceptance could contribute substantially to one’s enhanced state of emotional well-being. By acknowledging these shifts in emotionality and recognizing them as typical facets within the recovery journey, one allows for better navigation through one’s evolving affective landscape.
Recognizing Emotional Triggers
Recognizing the triggers that activate your emotions is a crucial initial step in overseeing your emotional health following weight loss surgery. Utilizing journaling as a method can be highly effective. Documenting how you feel during times of stress, sorrow, or anxiety can reveal recurring patterns and catalysts linked to detrimental eating habits.
Inquiring about what precisely instigated the emotion and pinpointing the specific feelings at that time is essential. Identifying these habitual responses is instrumental for controlling emotional eating and establishing more beneficial methods for coping, which are vital actions for sustaining emotional equilibrium post-surgery.
Developing Healthy Coping Mechanisms
Having pinpointed the emotional triggers that lead to your eating habits, it’s essential now to establish positive ways of dealing with them. Engaging in mindfulness can aid you in acknowledging and handling these triggers for emotional eating more adeptly. Techniques such as cognitive behavioral therapy and mindful eating require you to be fully conscious while dining, concentrating on selecting foods that are good for you. These methods strengthen your ability to cope emotionally and diminish nervousness during the transitional phase after weight loss surgery.
Even gentle physical activities like strolling have a notable effect on elevating your spirits and regulating stress levels. Delving into hobbies or artistic endeavors, such as sketching or painting, can offer valuable means for alleviating stress, too. Discovering new pastimes may also amplify sensations of achievement while steering attention away from food-centric thoughts.
Adopting strategies such as writing in a journal, meditating, exercising regularly, and pursuing creative ventures are all healthy approaches to coping with tension. Integrating these practices consistently into daily life assists in minimizing stress while nurturing one’s emotional wellness overall. It is beneficial, then, to pivot away from food-centered preoccupations towards alternative, satisfying pursuits that support a sounder emotional state.
Building a Strong Support System

Establishing a robust support network is crucial for coping with the emotional changes associated with weight loss surgery. Assistance from family, friends, or dedicated support groups can play an essential role in dealing with the emotional adjustments after shedding pounds surgically. Such supportive connections contribute to healthy conversations about self-image and acceptance, bolstering motivation and emotional health.
Participating in support groups or virtual communities provides a space where individuals on similar paths can share their experiences. Should you find yourself without close-knit backing, consider becoming part of a group that offers camaraderie to those seeking guidance. Embracing empathy towards oneself while reaching out for assistance is key when experiencing the emotive upheaval following your procedure.
Having access to a strong network of bariatric support peers can simplify your path post-surgery by minimizing stress and significantly enhancing your overall mental well-being throughout this journey.
Improving Body Image

Enhancing one’s self-perception is a vital part of the emotional evolution following weight loss surgery. Those who undergo such procedures may face concerns about their altered body image, shifts in lifestyle habits, and evolving interpersonal dynamics post-surgery. Common issues can include developing wrinkles on the face and experiencing sagging skin after shedding a considerable amount of weight. Despite this significant loss, individuals might still grapple with feelings associated with being overweight that can affect their sense of self.
The concept of body image encompasses your view regarding your own physical form, which can be shaped by myriad influences like cultural norms and personal history. Should struggles with body image become overwhelming, it’s important to seek assistance from medical professionals or support networks available to you. Documenting physical changes through photographs and measurements may serve as an effective method for enhancing morale.
Choosing attire that flatters your new shape and promotes confidence plays an essential role in fostering positive perceptions about oneself, both mentally and physically, and serves as a crucial step toward nurturing enhanced self-regard along with better overall health outcomes during this transformative journey.
Managing Relationship Dynamics
After undergoing weight loss surgery, individuals may find it difficult to navigate the complexities of relationship dynamics. The process can reveal challenges such as a lack of support from partners or feelings of resentment and jealousy, which often lead to tension in long-standing relationships. There is also an observed correlation between weight loss surgery and increased rates of divorce. To address these issues, it’s imperative for individuals to engage in open communication about the stressors they’re facing while also building a strong network for emotional support.
Securing assistance from counselors or participating in support groups can be pivotal for both partners dealing with the emotional changes post-surgery. These transformations might cause shifts in self-image and affect perceptions regarding how others view them. It’s essential to handle these transitions sensitively, ensuring that there is sufficient backing throughout this journey.
Finding Joy in New Hobbies

Discovering pleasure in new pastimes is an excellent strategy for enhancing emotional well-being following weight loss surgery. These hobbies act as a positive channel for the various emotions that surface throughout this transformative journey, offering substantial benefits to your emotional state and contributing to a sense of achievement.
Moving your attention away from food and towards engaging pursuits can greatly support emotional healing after weight loss surgery. Diving into different hobbies that delight you helps minimize stress and elevate your life’s overall enjoyment. Seize the chance to delve into fresh interests and enthusiasms as you cultivate a new lifestyle with beneficial health habits.
Setting Realistic Expectations
It’s essential to establish realistic expectations for outcomes after loss surgery to preserve a healthy body image and emotional state. Prior to embarking on weight loss surgery, it is important to anticipate the need for emotional adjustments in response to various potential results. Setting incremental, achievable objectives can promote ongoing motivation and feelings of accomplishment during the post-surgery phase.
Acknowledging minor victories throughout your weight loss journey can cultivate an optimistic attitude. Redirecting attention from physical attributes towards personal development aspects, such as enhanced self-esteem versus struggles with low self-esteem, encourages practicing kindness toward oneself and sustaining a positive emotional state during the process of losing weight, which contributes greatly to considerable weight reduction and successful outcomes. Adopting habits like savoring smaller meal portions aids this progression.
Keep in mind that success in this journey isn’t solely defined by scale numbers, but also encompasses one’s comprehensive mental and emotional well-being.
Seeking Professional Help
It is essential to seek support when emotional challenges become too much to handle alone. Professional counseling can help manage these issues and create efficient coping mechanisms both before and after surgery. Cognitive Behavioral Therapy (CBT) is particularly suggested for dealing with negative feelings and fostering a more positive self-perception after the operation. Before surgery, it’s important to know the top questions to ask your weight loss surgeon, such as details about the procedure, risks, and recovery.
Being mindful of your emotional health is critical, especially if you’re struggling with emotional changes after surgery. For many patients, professional counseling provides a pathway through tough periods while establishing a robust network of support. Never be reluctant to reach out for assistance when it’s necessary.
Wrapping It Up
Adjusting to emotional changes after weight loss surgery is just as important as the physical transformation. From navigating shifting self-image to managing evolving relationships, the journey requires patience, support, and self-compassion. Recognizing and addressing these emotional shifts can empower you to embrace the new version of yourself with confidence and resilience.
At Wellstar Comprehensive Bariatric Services, we understand that true success after bariatric surgery means supporting both your body and mind. Our dedicated team provides continued care and resources to help you feel emotionally prepared and supported at every stage of your journey. Whether you’re just beginning to explore options or are seeking a trusted weight loss surgeon in East Cobb, Marietta, Smyrna, Austell, LaGrange, or West GA, we’re here to guide you toward lasting, whole-person wellness. Let us walk with you on this life-changing path.
Frequently Asked Questions
What common emotional changes can I expect after weight loss surgery?
You can expect emotional ups and downs after weight loss surgery, such as agitation, anxiety, and even depression, as your body adjusts to the changes.
It’s important to be prepared for these feelings and reach out for support if needed.
How can I recognize my emotional triggers?
You can recognize your emotional triggers by journaling your feelings during stressful or anxious moments, which can reveal patterns and help you understand what sets off certain emotions.
This awareness is a key step in managing your responses effectively.
What are some healthy ways to cope with stress after weight loss surgery?
A great way to handle stress after weight loss surgery is to practice mindfulness and stay active.
Don’t forget to lean on your loved ones or join a support group for extra encouragement!
How can I improve my body image after weight loss surgery?
Improving your body image after weight loss surgery is all about embracing your progress—try taking photos to celebrate changes, wear outfits that make you feel great, and don’t hesitate to reach out to your support team if you’re struggling.
Remember, confidence is key!
When should I seek professional help for emotional challenges?
If your emotional challenges feel overwhelming, it’s important to seek professional help.
Therapy can be a great way to manage negative emotions and enhance your self-image.