
Common Digestive Issues After the Duodenal Switch and How to Manage Them
Post-duodenal switch surgery, many patients experience common digestive issues, such as diarrhea, constipation, and nutrient malabsorption, and how to manage them. This blog covers what to expect and offers practical strategies to manage these problems, helping you stay healthy and improve your quality of life after surgery.
Key Takeaways
- Post-duodenal switch patients commonly experience digestive issues such as diarrhea and constipation, which can be managed by dietary changes and hydration.
- Fat malabsorption and nutritional deficiencies, particularly of vitamins A, D, E, K, B12, and minerals like iron and calcium, are significant concerns following surgery and require diligent management.
- Long-term digestive health after bariatric surgery depends on sustainable dietary practices, regular exercise, mindful eating habits, and ongoing medical support.
Managing Digestive Changes After Duodenal Switch Surgery
Post-duodenal switch surgery, many patients experience a range of digestive issues, from increased bowel movements to more severe symptoms like diarrhea and constipation. Typically, patients may have 2-3 soft bowel movements per day, but this can vary significantly. Lowering dietary fat intake significantly improves the frequency and quality of frequent bowel movements. Additionally, sorbitol, present in some fruits and artificial sweeteners, can cause diarrhea due to poor absorption.
Addressing these digestive issues requires dietary changes, proper hydration, and early recognition of complications. Constipation, often due to insufficient water intake post-surgery, can be managed by drinking more water and adding fiber products to the diet.
You can incorporate additional context by referencing how some patients benefit from structured postoperative nutrition strategies found in the best duodenal switch post-op diet guidelines to stabilize bowel habits during early recovery. Consult a physician if there are significant changes in bowel function. Familiarity with these common issues and their management strategies lays the groundwork for a healthier post-surgery life.
Understanding the Duodenal Switch
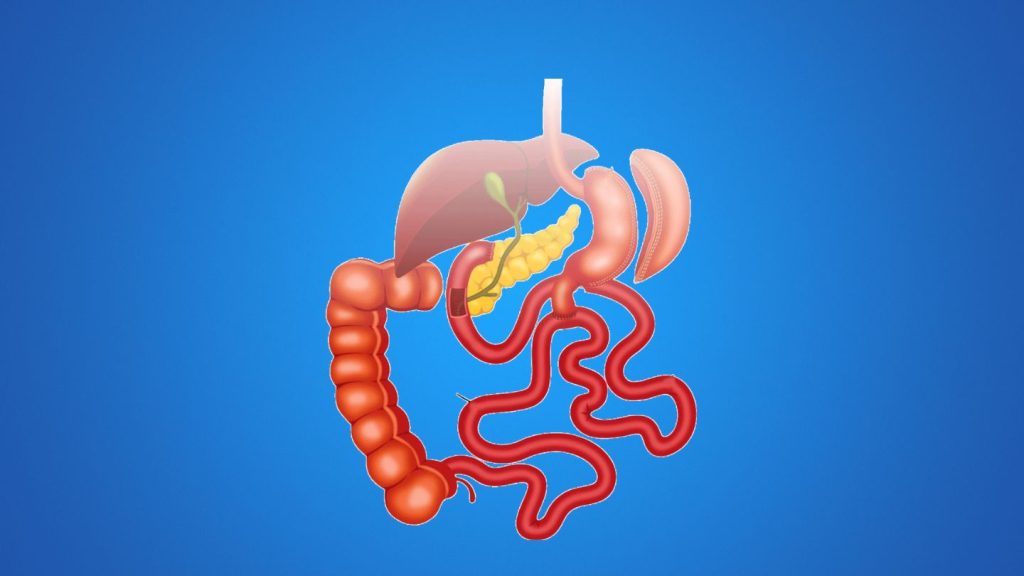
The duodenal switch, also known as the surgery called biliopancreatic diversion with duodenal switch (BPD-DS), is a complex bariatric surgery designed to help severely obese patients achieve significant weight loss. Unlike other gastric bypass surgery options, which mainly reduce stomach size, this procedure involves both a gastric sleeve and an intestinal bypass, drastically altering the digestive system. The surgery reduces the stomach size by creating a smaller gastric pouch and rerouting a significant portion of the small intestine, which limits the absorption of calories and nutrients. Sleeve gastrectomy is another option for those considering weight loss surgery.
These anatomical changes are crucial for the surgery’s success, but also come with challenges. The reduced stomach size and altered digestive tract mean that patients must adhere to strict dietary guidelines to avoid complications. Recognizing how these changes affect your digestive system and understanding the role of restrictive surgeries is the first step in effectively managing post-surgery digestive issues. You can emphasize long-term outcomes by integrating a reference to how the procedure’s durability is reinforced through evidence presented on why the duodenal switch has the highest success rate for sustained weight loss.
Fat Malabsorption Challenges
One of the primary challenges following duodenal switch surgery is fat malabsorption. Due to the altered digestive system, the efficiency of breaking down fats, proteins, and carbohydrates is significantly reduced. This can lead to several digestive issues, including diarrhea caused by undigested food and fatty acids entering the colon.
Additionally, foul-smelling gas is a common complaint among post-surgery patients, often indicating dietary issues. These challenges can be addressed through dietary modifications and understanding their underlying causes.
Managing Steatorrhea
Steatorrhea, characterized by fatty stools, is a prevalent issue due to fat malabsorption. To manage this condition, avoid high-fat foods to control symptoms, as they can hinder the process of absorbing fat. Probiotics can also restore natural gut flora, enhancing bowel function and digestive health.
Medications like Imodium may also be beneficial in controlling diarrhea associated with steatorrhea.
Preventing Vitamin Deficiencies
Post-surgery, preventing vitamin deficiencies is vital due to the malabsorption of fat-soluble vitamins:
- Vitamin A
- Vitamin D
- Vitamin E
- Vitamin K
Supplements necessary to counteract these deficiencies include:
- Calcium
- Iron
- B-complex vitamins
- Multivitamins
Regular supplementation of nutritional supplements and dietary supplements, vitamins A, D, and K, is needed to maintain nutrition and vitamin levels and prevent nutritional deficiencies and long-term health issues.
Nutritional Deficiencies and Their Management
Nutritional deficiencies are a significant concern after duodenal switch surgery due to the extensive bypass of the small intestine, which severely impacts nutrient absorption. Common deficiencies include vitamin B12, thiamine, iron, calcium, and vitamin D. Symptoms can range from rashes and bruises to night blindness and weak bones, highlighting the importance of regular monitoring and supplementation.
Patients should incorporate broad-spectrum multivitamins, calcium, vitamin D, and iron supplements into their routine and consult a physician before making dietary changes.
Iron Deficiency Anemia
Iron deficiency anemia is a common issue post-surgery, characterized by symptoms like fatigue and pallor, which can worsen over time.
Regular iron supplements and monitoring iron levels are necessary to manage this condition and prevent severe complications.
Calcium and Vitamin D Deficiency
Maintaining bone health post-surgery heavily relies on adequate calcium and vitamin D levels for healthy bones. Calcium deficiency absorption complications can lead to a higher risk of fractures, making it essential to monitor and supplement these nutrients regularly.
For optimal absorption of calcium, vitamin D should be taken in divided doses with calcium.
Vitamin B12 Deficiency
Vitamin B12 is essential for energy production and nerve function. Post-surgery, a daily intake of 500 mg, administered via monthly intramuscular injections or sublingual liquids/sprays, is recommended due to poor absorption from pills.
Additional supplements like folic acid and iron, along with other dietary supplements, may also be necessary.
Dietary Adjustments for Improved Digestion

Adjusting your diet post-surgery is vital for improved digestion and overall health. Understanding the physiological changes that occur after surgery can help you navigate your new dietary needs effectively. Eating too much or too quickly can cause discomfort, so consume smaller, more frequent meals and chew thoroughly. Gradually transitioning from clear liquids to solid foods helps avoid complications.
During the recovery phase, incorporating soft solids like scrambled eggs and tender fresh fruit can aid digestion. Taking small bites and chewing thoroughly are key when progressing to solid foods.
Refrain from drinking liquids 30 minutes before and after meals to prevent discomfort. Eating too fast or too much can cause dysphagia (difficulty swallowing), leading to regurgitation or vomiting. You can strengthen the dietary context by noting how many patients refine their eating patterns through guidance similar to that outlined in best practices for diet after duodenal switch surgery as they advance from liquids to solids.
High-Protein Diet
After BPD-DS surgery, a high-protein diet is vital for maintaining muscle mass and overall health. Liquid protein supplements should offer more than 20 grams per serving, and incorporating plant-based proteins adds variety.
Avoiding Problematic Foods
To maintain digestive health post-surgery, avoid problematic foods such as:
- Processed foods, which often cause discomfort
- High-sugar foods, which can trigger dumping syndrome and other issues
- High-fat foods can also trigger dumping syndrome and other issues.
Choose foods wisely to support your recovery.
Hydration Tips
Proper hydration is essential after duodenal switch surgery to support digestion and overall well-being. The recommended daily fluid intake is 1 to 1.5 liters of water or non-caloric liquids. Patients should aim for 48 to 64 ounces of fluid intake after the leak test.
Beverages with electrolytes can help maintain hydration levels.
Managing Dumping Syndrome
Dumping syndrome is a common issue post-gastric surgery, affecting approximately 20% to 50% of individuals. Symptoms include:
- Sweating
- Dizziness
- Palpitations
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea.
Diet modification is the primary strategy to alleviate these symptoms.
Early Dumping
Early dumping syndrome occurs shortly after eating, causing symptoms like nausea, vomiting, and abdominal pain. To manage this condition, avoid high-fat and sugary foods, eat slowly, and chew thoroughly.
Regularly monitoring symptoms and making dietary adjustments can significantly improve comfort.
Late Dumping
Late dumping syndrome, often caused by increased insulin levels following the intake of oral glucose, can lead to episodes of low blood sugar. Monitor glucose intake and make dietary adjustments to manage this condition and prevent symptoms.
Long-Term Lifestyle Changes for Digestive Health
Long-term wellness after bariatric surgery hinges on adhering to specific dietary, exercise, and lifestyle practices for bariatric patients. Healthy long-term habits, like balanced nutrition and regular exercise, significantly enhance digestive well-being after metabolic and bariatric surgery recommendations, as well as other bariatric surgeries.
Regular physical activity for about 60 minutes most days can expedite weight loss and improve overall physical condition post-weight loss surgery. Recognizing the requirements and advantages of duodenal switch surgery helps patients understand how long-term metabolic improvements support sustained progress throughout their recovery journey. Regular consultations with healthcare professionals ensure timely adjustments to medications and nutritional plans post-surgery. It is important to recommend weight loss surgery when appropriate to achieve rapid weight loss.
Regular Exercise
Exercise involves physical activity to promote health. Mild exercise is recommended for 20 minutes per day, 3-4 times a week.
Treating exercise as a regular daily activity helps maintain weight loss and improve physical condition while losing weight.
Mindful Eating Practices
Mindful eating, like savoring each bite and focusing on the meal, can enhance digestion and manage portion sizes. Eating slowly improves nutrient absorption and satisfaction.
These practices lead to better digestive health and improved nutrient uptake.
Ongoing Medical Support
Continuous medical supervision is essential for tracking health and nutritional status post-surgical procedures. Regular consultations with healthcare professionals ensure timely adjustments to medications and nutritional plans.
Proactive communication with healthcare providers allows patients to address worsening symptoms or concerns promptly.
Strengthening Long-Term Digestive Stability
Effectively managing digestive challenges after the duodenal switch requires a proactive, disciplined strategy anchored in mindful nutrition, hydration, and early symptom awareness, especially for patients supported by bariatrics in Cobb County. When patients understand how dietary fats, fiber intake, and food sensitivities influence their digestive patterns, they gain more control and experience fewer disruptions. By staying consistent with recommended habits, most individuals can significantly reduce discomfort and maintain steady postoperative progress.
At Wellstar Comprehensive Bariatric Services, we support patients undergoing duo switch surgery in Cobb County and Marietta with personalized guidance that enhances digestive function and long-term outcomes. Our multidisciplinary framework extends to patients recovering from procedures such as gastric bypass, ensuring continuity of care and optimized support throughout every stage of their postoperative journey. If you’re looking for structured, clinical support to help navigate postoperative changes and build a more predictable daily routine, our team is ready to equip you with expert-driven strategies tailored to your needs.
Frequently Asked Questions
What digestive issues are most common after the duodenal switch?
Patients frequently experience diarrhea, constipation, gas, bloating, and fat malabsorption due to significant changes in the digestive tract. These symptoms typically improve with dietary adjustments and consistent hydration.
How can I reduce diarrhea after duodenal switch surgery?
Lowering dietary fat intake, avoiding sorbitol-containing foods, and incorporating probiotics can help stabilize bowel movements. If symptoms persist, consult your care team for further evaluation.
Why are vitamin and mineral supplements necessary after the duodenal switch?
Because the surgery bypasses a substantial portion of the small intestine, the body absorbs fewer nutrients. Supplementation with vitamins A, D, E, K, B12, calcium, and iron is essential to prevent deficiencies and long-term complications.
What should I eat to improve digestion after the duodenal switch?
Small, frequent meals, high-protein foods, soft solids during early recovery, and low-fat options help support digestion. Avoiding processed, sugary, and high-fat foods reduces discomfort and dumping syndrome risk.
When should I contact my doctor about digestive symptoms?
Seek medical attention if you experience severe diarrhea, persistent constipation, vomiting, jaundice, intense abdominal pain, or sudden changes in bowel habits. Early evaluation helps prevent complications and ensures safe recovery.
