Why Duodenal Switch Has the Highest Success Rate for Long-Term Weight Loss
The dual switch has revolutionized long-term weight loss by offering unparalleled success rates compared to other procedures. This innovative surgery combines two powerful mechanisms that promote sustained weight loss and improve overall health. Unlike other methods, it addresses both restrictive and malabsorptive aspects, ensuring more effective results. Patients often experience not just significant weight loss but also lasting improvements in conditions like diabetes and high blood pressure. In this blog, we’ll explore what makes the dual switch so effective, its impressive long-term success rates, and the additional health benefits it can provide.
Key Takeaways
- Duodenal switch surgery combines sleeve gastrectomy and intestinal bypass techniques, significantly reducing food intake and calorie absorption, making it one of the most effective bariatric procedures.
- Patients often achieve and maintain remarkable long-term weight loss, with studies showing that 70% sustain at least 50% of their excess weight loss for over a decade.
- Beyond weight loss, duodenal switch surgery leads to improvements in metabolic health, with many patients experiencing remission of conditions like type 2 diabetes and reductions in cholesterol and hypertension.
Understanding Duodenal Switch Surgery
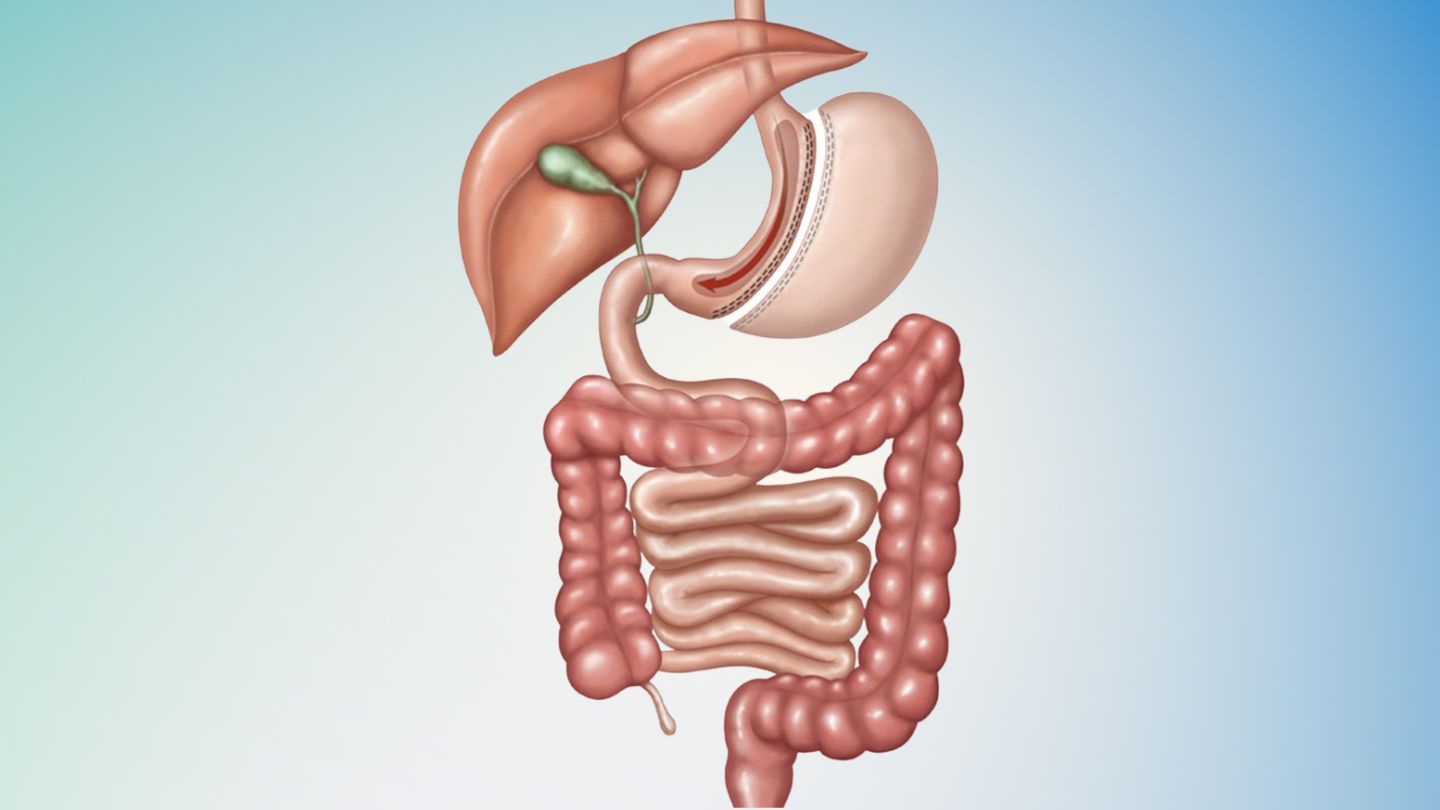
Duodenal switch surgery, also known as biliopancreatic diversion with duodenal switch, is a complex weight loss procedure designed to promote significant weight loss and enhance overall health. This surgery combines two primary techniques: Sleeve gastrectomy and intestinal bypass. During the Sleeve Gastrectomy component, approximately 80% of the stomach is removed, leaving a tube or sleeve-shaped stomach that reduces food intake. This smaller stomach helps patients feel full sooner and eat less.
The intestinal bypass portion of the surgery involves rerouting the small intestine to decrease nutrient absorption. Specifically, the middle segment of the small intestine is closed off, and the last part is connected directly to the duodenum. This bypass means that food bypasses a significant portion of the digestive tract, leading to fewer calories and nutrients being absorbed. Combining these two elements, the dual switch reduces both the volume of food consumed and the number of calories absorbed, making it a highly effective weight loss surgery.
Unlike traditional open surgery, the duodenal switch procedure is typically performed using minimally invasive techniques, which reduce recovery time and the risk of complications. Bariatric surgeons often recommend duodenal switch surgery for patients who have struggled with severe obesity and have not had success with other weight loss methods.
Understanding the mechanics of this surgery allows patients to appreciate why it stands out among other bariatric procedures.
Mechanism of Weight Loss in Duodenal Switch
Duodenal switch surgery facilitates weight loss by simultaneously reducing the amount of food one can eat and diminishing calorie absorption. By surgically removing a substantial part of the stomach, it restricts how much food can be ingested at once, resulting in decreased caloric intake. The procedure involves an intestinal bypass that drastically lowers nutrient absorption area, aiding in nutrient absorption. In losing weight, fewer calories are absorbed.
The success of duodenal switch surgery is also significantly influenced by hormonal alterations post-operation. The level of ghrelin – a hormone responsible for signaling hunger – typically drops sharply following this surgery. This decrease assists in curbing appetite and minimizes eating desires. Levels of GLP-1 tend to increase. This hormone plays a role in suppressing appetite and enhancing blood sugar regulation. Together these hormonal changes not only facilitate significant weight loss but also contribute positively to metabolic health.
When considering its ability to alter both hunger hormones and metabolic functions effectively, the duodenal switch stands out as one of the top-performing procedures among common weight loss surgeries — combining traits from both gastric sleeves and gastric bypass interventions leading to more pronounced outcomes concerning shedding excess pounds.
Individuals who opt for this type of surgical intervention Observe swift progress on their journey toward slimming down within 12 to 18 months after their operation while persisting with efforts focused on long-term maintenance conducive to continued success at losing unwanted additional body mass.
Long-Term Success Rates of Duodenal Switch
When it comes to long-term success rates, the duodenal switch surgery stands out among bariatric procedures. Studies have shown that patients typically achieve an average long-term weight loss of 70% of their excess body weight over a decade. This is a remarkable achievement, especially when compared to other weight loss surgeries. Around 90% of patients manage to lose at least 50% of their excess weight, underscoring the effectiveness of this procedure.
The initial phase after duodenal switch surgery is characterized by rapid weight loss, with patients often losing a significant portion of their excess weight within the first 12 to 18 months. On average, patients can achieve up to 80% of their excess weight loss within two years of the surgery. This rapid reduction in weight not only boosts patient morale but also leads to early improvements in obesity-related conditions.
One of the most compelling advantages of duodenal switch surgery is its ability to maintain long-term weight loss. Studies indicate that patients who undergo this surgery retain a higher percentage of their weight loss compared to those who have had other forms of bariatric surgery.
Approximately 70% of patients maintain their weight loss for ten years or longer. This sustained success is a testament to the surgery’s effectiveness and why many bariatric surgeons recommend duodenal switch surgery for individuals seeking long-term weight management solutions.
Benefits Beyond Weight Loss
Before:
The objective of duodenal switch surgery extends well beyond mere weight reduction. One key benefit is the positive effect it has on metabolic health, particularly for those suffering from type 2 diabetes. A considerable number of patients find themselves in remission from diabetes following the procedure, which often allows them to lower their use or completely stop taking their diabetes medications. This operation frequently leads to a decrease in high cholesterol and blood pressure levels, contributing to improved overall wellness.
After:
Substantial weight loss remains one prime aim of duodenal switch surgery, but its advantages stretch much wider than simply losing pounds. Notable benefits include:
- Enhanced metabolic health is especially beneficial for people with type 2 diabetes.
- Frequent remissions post-surgery allow many individuals to diminish or halt their intake of diabetes medication altogether.
- Marked reductions in both high cholesterol and hypertension that bolster general health.
Compared to other weight loss surgeries, the duodenal switch offers superior efficacy against various conditions associated with obesity, such as significant amelioration in sleep apnea along with additional respiratory complications prevalent among those struggling with severe obesity. The consequential improvement permits greater engagement in physical activities and mental well-being thereby enriching life quality substantially.
Such enhancement across facets of physical and psychological welfare serves as testamentary evidence that positions duodenal switch procedures as transformationally impactful interventions within patient lives dealing with excessive weight issues.
Candidate Criteria for Duodenal Switch

To ascertain who is an appropriate candidate for duodenal switch surgery, specific criteria must be met. Individuals with a Body Mass Index (BMI) of at least 50 or those experiencing severe conditions related to obesity are typically given priority for the procedure. Although the baseline BMI criterion usually exceeds 40, patients suffering from obesity-related health issues such as diabetes or hypertension could also qualify if their BMI stands at 35.
Before qualifying for duodenal switch surgery, candidates should have already tried and been unsuccessful in achieving weight loss through conventional means like dieting and exercising. This stipulation ensures that the procedure is seen as a last resort option after other methods fail to produce results. Thorough psychological screening forms part of the evaluation process to determine whether individuals are adequately prepared mentally to handle substantial lifestyle modifications following the operation.
The meticulous vetting protocol encompasses additional medical assessments along with expert consultations aimed at gauging overall surgical suitability. Pre-surgery preparations often include adhering to a liver-reduction diet, among other steps taken to improve patient health prior to surgery. Through this rigorous selection process, bariatric surgeons aim toward enhancing postoperative success rates and securing enduring outcomes when it comes to long-term weight management.
Read More: Best Practices for Diet After Duodenal Switch Surgery
Recovery and Follow-Up Care
Following a duodenal switch surgery, patients undergo a progressive dietary shift from liquid to solid intake. Initially consuming clear liquids, they gradually incorporate pureed and soft foods over the first-month post-operation. This gradual food reintroduction allows the digestive system to adjust properly while minimizing potential complications. In the initial three months following surgery, individuals often experience significant weight loss of about half a pound to one pound daily, providing considerable encouragement.
To avoid nutritional deficiencies that are frequently associated with duodenal switch procedures, ongoing monitoring, and supplementation are mandatory for patients. A strict adherence to prescribed vitamin and mineral supplements is imperative for sustained well-being. Regular follow-up visits are scheduled at intervals of 1 month, 3 months, and 6 months, followed by annual check-ups, ensuring close tracking of patient progress and timely intervention when necessary.
Postoperative recovery involves sufficient rest as well as abstaining from strenuous physical activities during the early weeks after surgery. Light walking is recommended in order to promote blood flow and decrease clotting risks. Depending on the level of exertion required for the job, most patients find themselves capable of returning to their professional roles within a two-week time period.
Comparisons with Other Weight Loss Surgeries

When the duodenal switch surgery is measured against other weight loss procedures, such as gastric bypass and sleeve gastrectomy, its distinctive benefits become evident. The duodenal switch results in a more substantial decrease in body mass index (BMI) over the long term than the Roux-en-Y gastric bypass, averaging an extra reduction of 6.2 BMI units. Within two years following the operation, patients can expect to shed up to 80% of their surplus weight, positioning it as one of the most effective options for surgical weight loss.
The dual approach of restriction and malabsorption employed by the duodenal switch yields more considerable weight reductions compared with either gastric bypass or sleeve gastrectomy alone. Although Roux-en-Y gastric bypass holds popularity due to its shorter duration—approximately two hours—the longer four-hour procedure of a duodenal switch is often suggested for individuals presenting with higher levels of obesity. This intricate interplay between restrictive and malabsorptive techniques underpins why this particular surgery delivers superior outcomes regarding shedding pounds.
For those who have undergone numerous surgeries without achieving their desired results from traditional methods like gastric bypass or Sleeve interventions, opting for a duodenal switch could present significant advantages, especially in terms of maintaining weight loss over time. Considering these distinctions gives people struggling with severe obesity crucial insights that assist them in determining which surgical route might offer them optimal success on their journey toward meaningful long-term health improvements through sustained excess weight reduction.
Transform Your Health with Duodenal Switch Surgery
The duodenal switch surgery remains one of the most effective solutions for sustainable long-term weight loss, offering unmatched success rates among bariatric procedures. Combining sleeve gastrectomy and intestinal bypass techniques addresses both restrictive and malabsorptive aspects, ensuring significant and lasting weight reduction. Beyond weight management, it delivers profound health benefits like remission of type 2 diabetes and improved cholesterol and blood pressure levels, enhancing overall quality of life. Its ability to provide consistent results over the years makes it the preferred choice for those battling severe obesity.
At Wellstar Comprehensive Bariatric Services, we specialize in delivering expert-led bariatric care, including duo switch surgery in Marietta. With a focus on state-of-the-art techniques and personalized attention, we are dedicated to helping you achieve your health goals. Our weight loss surgeons in East Cobb will guide you through every step of the process, ensuring your safety, comfort, and long-term success. Take the first step today by scheduling a consultation with us to experience the life-changing benefits of this transformational procedure.
FAQs About Duodenal Switch Surgery
What is duodenal switch surgery?
Duodenal switch surgery combines sleeve gastrectomy and intestinal bypass to reduce food intake and calorie absorption. It’s a bariatric procedure designed to achieve significant and long-lasting weight loss, along with metabolic health benefits.
Who is a good candidate for duodenal switch surgery?
Candidates typically have a BMI of 50 or higher or a BMI over 35 with obesity-related health issues. They should have tried other weight loss methods unsuccessfully and undergo thorough medical and psychological evaluations.
What are the long-term benefits of the procedure?
Beyond weight loss, the surgery often results in improved metabolic health, diabetes remission, lower cholesterol, and reduced hypertension. It also enhances quality of life by alleviating obesity-related conditions like sleep apnea.
How does recovery from duodenal switch surgery work?
Patients start with a liquid diet, gradually transitioning to solid foods. Recovery includes rest, light walking, and regular vitamin supplementation. Follow-up care includes scheduled check-ups to track progress and manage potential complications.
How does the duodenal switch compare to other bariatric surgeries?
It offers greater long-term weight loss and health benefits than gastric bypass or sleeve gastrectomy by combining restrictive and malabsorptive techniques. It’s particularly effective for individuals with severe obesity or previous unsuccessful surgeries.
