
The Complete Guide to Bariatric Surgery: Everything You Need to Know
Bariatric surgery is a powerful medical solution for individuals struggling with severe obesity and related health risks. It supports significant, long-term weight loss by altering the digestive system to reduce food intake or absorption. Beyond weight control, it helps improve conditions like diabetes, high blood pressure, and sleep apnea. Proper preparation, ongoing lifestyle changes, and professional medical guidance are essential for success. In this blog, we explore how bariatric surgery works, who qualifies, key procedures, and what to expect before and after the operation.
Key Takeaways
- Bariatric surgery is a surgical intervention aimed at significant weight loss for individuals with severe obesity, especially when traditional methods fail.
- There are several types of bariatric procedures, including gastric bypass, sleeve gastrectomy, and duodenal switch, each with unique benefits and recovery considerations.
- Successful long-term outcomes after bariatric surgery hinge on a commitment to lifestyle changes, including diet, exercise, and ongoing medical support to mitigate risks and enhance health.
Understanding Bariatric Surgery
Bariatric surgery is a surgical solution designed to combat severe obesity and the numerous health issues that accompany it. The primary goal of bariatric surgery is to modify the stomach and intestines to facilitate significant weight loss and improve overall health. This type of surgery is often considered when traditional methods like diet and exercise have not resulted in lasting weight loss, especially for those with a Body Mass Index (BMI) of 40 or higher, or 35 with obesity-related health conditions.
A bariatric surgeon alters the digestive system to help limit food intake and reduce calorie absorption, making bariatric surgery an effective tool in the fight against obesity. For patients wondering about timing, knowing how quickly you can get bariatric surgery can clarify the typical evaluation steps and scheduling process.
Candidates for bariatric surgery are typically those who face serious health risks due to obesity and have not achieved long-term success with other weight loss methods. Exploring whether I am eligible for bariatric surgery offers clear criteria to help determine if I meet the medical and lifestyle requirements for surgery. The surgery is usually performed after thorough evaluations to ensure the patient’s readiness and suitability for the procedure.
Types of Bariatric Surgery Procedures
There are several types of bariatric surgery procedures, each with unique approaches and benefits. These include gastric bypass surgery, sleeve gastrectomy, and the duodenal switch. Each procedure varies in complexity, recovery time, and the extent of weight loss expected, including weight loss surgeries.
Evaluating these different options helps determine the best approach to address severe obesity and associated health issues. Gaining clarity on the different types of bariatric surgery provides insight into which procedure aligns best with your medical needs and lifestyle goals.
Gastric Bypass Surgery
Gastric bypass surgery, also known as the Roux-en-Y procedure, involves:
- Creating a smaller stomach pouch to significantly reduce food intake.
- Connecting this pouch directly to the small intestine bypasses a substantial portion of it, which decreases the absorption of calories and nutrients.
- Using a laparoscopic approach, refined since 1993, that involves small incisions and less recovery time, making it a minimally invasive option.
Patients who undergo gastric bypass surgery often experience rapid weight loss and improved health conditions.
This procedure is particularly beneficial for those with severe obesity and related health issues such as type 2 diabetes and gastroesophageal reflux disease (GERD) and acid reflux. Significantly limiting food intake and altering the digestive process helps patients lose a substantial amount of excess weight, often resulting in a transformative weight loss journey within the digestive tract.
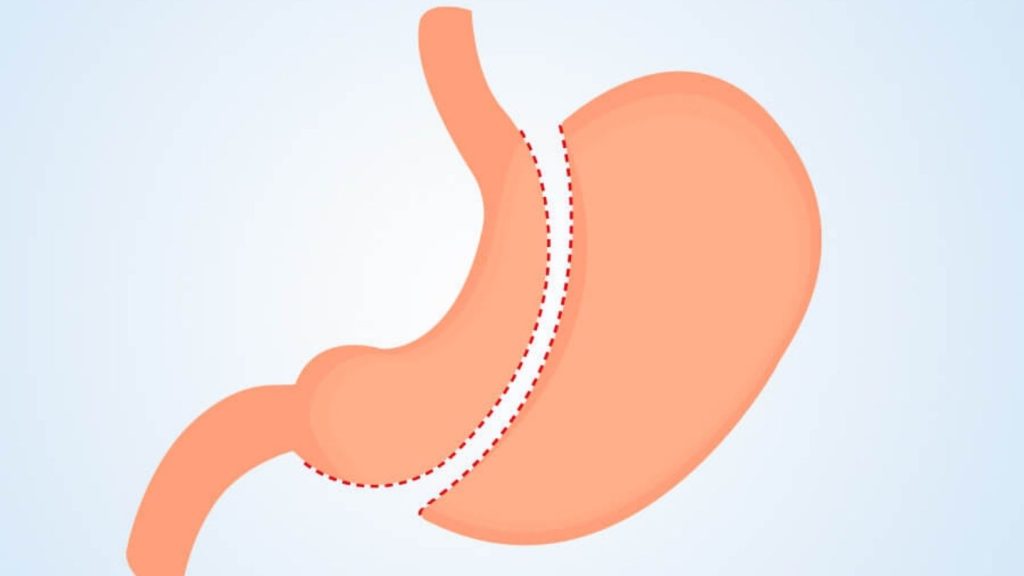
Sleeve Gastrectomy
Sleeve gastrectomy is another popular bariatric procedure that involves:
- Removing about 75-80% of the stomach, leaving a banana-shaped section that holds less food.
- Limiting food intake due to the reduced stomach size.
- Decreasing appetite and increasing feelings of fullness.
The procedure is less complex than other bariatric surgeries, making it a preferred choice for many patients.
A significant advantage of sleeve gastrectomy is its effectiveness in promoting weight loss while maintaining a lower complication rate and straightforward recovery. Patients who undergo this gastric sleeve procedure often see substantial weight loss and improvements in obesity-related conditions such as sleep apnea and type 2 diabetes.
Duodenal Switch
The duodenal switch procedure is a combination of sleeve gastrectomy and intestinal bypass. Initially, a sleeve gastrectomy is performed, followed by dividing the duodenum and bypassing approximately 75% of the small intestine. This combination leads to decreased calorie absorption and significant hormonal changes that aid in weight loss, including biliopancreatic diversion with duodenal switch.
This procedure is particularly effective for those needing to lose a substantial amount of weight and who may have not seen success with other bariatric surgeries. The duodenal switch also helps avoid complications such as dumping syndrome, making it a viable long-term solution for severe obesity. Additionally, the duodenal switch BPD DS is an option for those seeking effective weight loss solutions.
Benefits of Bariatric Surgery

Bariatric surgery offers numerous health benefits, including:
- A significant reduction in the incidence of type 2 diabetes.
- Improved cardiovascular health.
- Better blood sugar control.
- A dramatic decrease in hunger.
- Improved metabolic health through metabolic and bariatric surgery.
These benefits are particularly advantageous for those struggling with obesity-related health conditions.
Beyond physical health benefits, bariatric surgery enhances overall quality of life. Patients often report increased energy levels, reduced joint pain, and improvements in sexual function and self-confidence. Addressing the most common bariatric surgery myths can help dispel misconceptions and ensure individuals approach the procedure with accurate expectations and confidence. These changes contribute to a happier, more active lifestyle, allowing individuals to engage more fully in daily activities and social interactions.
Long-term benefits of bariatric surgery include sustained weight loss, transformed bodies, and restored health. Many patients experience a resolution of obesity-related health conditions, leading to a healthier and more fulfilling life. The surgery not only addresses physical health issues but also brings about significant emotional and psychological improvements.
Preparing for Bariatric Surgery
Preparing for bariatric surgery involves thorough assessments of heart and lung function to ensure the patient is fit for surgery. A psychological evaluation is also necessary to determine the patient’s readiness for the significant lifestyle changes required post-surgery. These evaluations ensure the patient is physically and mentally prepared for the challenges ahead.
Patients must adopt positive health behaviors well before surgery, such as:
- Quitting smoking, which is especially important to prevent complications during and after the procedure
- Improving sleep habits
- Engaging in educational sessions about the bariatric surgery process and the necessary lifestyle changes to better understand what to expect and how to prepare
Patients should also consult their health insurance or Medicare/Medicaid to verify coverage for bariatric surgery. This step ensures there are no unexpected financial burdens and allows the patient to focus fully on their weight loss journey. Strengthening your readiness with resources like preparation for bariatric surgery can help create a detailed plan that supports long-term success. Commitment to a weight loss and exercise regimen is also crucial for success, starting well before the bariatric surgery requirements.
Post-Surgery Recovery and Care

Recovery after bariatric surgery follows a structured diet progression:
- Start with a liquid-only diet for the first few weeks.
- Transition to pureed foods.
- Move on to soft foods.
- Eventually resume regular food consumption about six to eight weeks post-surgery.
Drinking sufficient fluids throughout the day is essential, especially during the initial recovery phase.
Post-surgery care includes:
- Vitamin and mineral supplementation due to reduced nutrient absorption capacity.
- Regular follow-up visits and medical checkups to monitor health progress and address complications such as dumping syndrome or nutritional deficiencies.
- Gradual introduction of new foods to identify any that may cause discomfort or adverse reactions.
Long-term follow-up plans, including nutritional, lifestyle, and medical condition tracking, are necessary for sustained success. A support system can help patients navigate post-surgery challenges and maintain their weight loss journey.
Long-Term Success and Lifestyle Changes
Achieving long-term success after bariatric surgery requires a steadfast commitment to a healthy lifestyle. This includes:
- Making permanent changes to one’s diet
- Engaging in regular exercise
- Staying hydrated by consuming over 64 ounces of fluid daily
- Maintaining a daily protein intake of 60 to 100 grams to prevent weaknesses and muscle loss
Key recommendations for sustained weight loss and overall health improvement include healthy eating and regular physical activity. For some patients considering future flexibility, understanding whether bariatric surgery can be reversed is important when weighing the permanence of different procedures. Weight loss tips include:
- Healthy eating and regular physical activity
- Lifelong nutritional supplements and mineral supplementation to avoid severe health complications and ensure the body receives all essential nutrients
- Participation in support groups and seeking continuous support to maintain a healthier lifestyle while focusing on losing weight.
The likelihood of achieving long-term success and improvement in obesity-related health conditions is significantly higher with bariatric surgery compared to non-surgical interventions. Commitment to these lifestyle changes can lead to a better quality of life and improved mental health.
Moving Forward with Confidence
Bariatric surgery offers a transformative path for individuals facing severe obesity, addressing both weight-related health risks and overall quality of life. With procedures designed to aid significant and sustainable weight loss, this medical solution can reduce complications like diabetes and hypertension. Success depends on thorough preparation, personalized care, and a commitment to long-term lifestyle changes that support lasting results.
At Wellstar Comprehensive Bariatric Services, we provide expert care and personalized treatment plans for those considering bariatric surgery in East Cobb, Marietta, Smyrna, LaGrange, West GA, and Austell. Our team is ready to guide you from initial consultation through recovery and beyond, helping you achieve improved health and a renewed sense of well-being. Contact us to begin your journey toward a healthier future.
Frequently Asked Questions
Who is an ideal candidate for bariatric surgery?
An ideal candidate typically has a Body Mass Index (BMI) of 40 or higher, or a BMI of 35 or more with serious obesity-related health conditions like type 2 diabetes or hypertension. Candidates should have attempted weight loss through diet and exercise without lasting success and be ready for significant lifestyle changes.
How long does it take to recover after bariatric surgery?
Initial recovery usually takes four to six weeks, but full adjustment to new eating habits and energy levels can take several months. Patients follow a structured diet progression, liquids, pureed foods, and soft foods before returning to a regular diet while attending regular medical checkups.
What are the most common types of bariatric surgery?
The most common procedures include gastric bypass, sleeve gastrectomy, and duodenal switch. Each offers different approaches to reducing food intake and absorption, and the right option depends on individual health needs, weight-loss goals, and your surgeon’s recommendations after a thorough evaluation.
What lifestyle changes are required after the procedure?
Long-term success requires permanent lifestyle changes. Patients must maintain a balanced, nutrient-rich diet, consume 60–100 grams of protein daily, drink at least 64 ounces of fluid, take lifelong vitamin and mineral supplements, and engage in regular physical activity to maintain weight loss and overall health.
Will health insurance cover bariatric surgery?
Many insurance providers, including Medicare and Medicaid, cover bariatric surgery if medical necessity is proven. Coverage requirements often include documented attempts at weight loss and a physician’s recommendation. Checking with your insurer early ensures clarity about pre-approvals and potential out-of-pocket costs.
