
A Comprehensive Guide to Gastric Bypass Surgery
Gastric bypass surgery is a proven medical option for individuals seeking significant and sustained weight loss. This procedure helps reduce stomach size and reroute the digestive tract to limit calorie absorption, improving overall health. It can also alleviate conditions such as diabetes, high blood pressure, and sleep apnea. Careful preparation and ongoing lifestyle changes are essential for long-term success. In this blog, we outline the procedure, key benefits, potential risks, and what to expect before and after surgery.
Key Takeaways
- Gastric bypass surgery, specifically the Roux-en-Y procedure, aims to facilitate significant weight loss by creating a smaller stomach pouch that bypasses much of the stomach and small intestine.
- Candidates must meet specific BMI criteria and undergo thorough evaluations to ensure their readiness for lifestyle changes, with insurance coverage often playing a crucial role in the surgical journey.
- Post-surgery, patients must commit to a structured nutrition and exercise plan, adhere to follow-up care, and seek emotional support to enhance their recovery and maintain long-term weight loss success.
Understanding Gastric Bypass Surgery
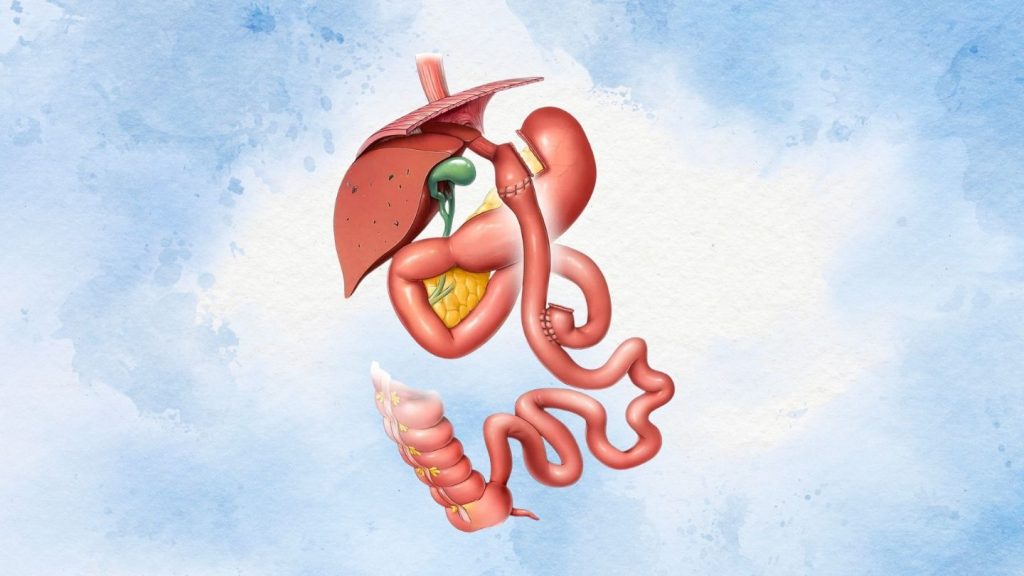
Gastric bypass surgery, commonly known as Roux-en-Y, is a type of weight loss surgery designed to help patients achieve significant weight loss. The primary goal of this bariatric surgery is to create a smaller stomach pouch that connects directly to the small intestine, bypassing most of the stomach and the first part of the small intestine. This alteration in the digestive system allows patients to absorb fewer calories, leading to substantial weight loss.
Patients undergoing gastric bypass surgery can expect to lose approximately how much of their excess weight within two years following the procedure. This remarkable weight loss can significantly improve or resolve various obesity-related health conditions such as type 2 diabetes, high blood pressure, and gastroesophageal reflux disease (GERD). However, potential candidates must understand both the benefits and risks associated with gastric bypass surgery to make an informed decision.
The success of gastric bypass surgery depends on a patient’s commitment to long-term lifestyle changes, including healthy eating habits and regular physical activity. Adhering to these changes helps patients maintain their weight loss and improve their overall health.
Grasping the intricacies of this metabolic and bariatric surgery marks the beginning of a successful weight loss journey. Patients weighing different bariatric options benefit from understanding gastric bypass surgery vs gastric sleeve, which gives knowledge on how each procedure impacts weight loss results, nutrient absorption, and long-term lifestyle considerations.
Qualifications for Gastric Bypass Surgery
Candidates for gastric bypass surgery must meet specific criteria and undergo a thorough screening process. A recommendation from a qualified healthcare provider is required, and patients typically have to meet specific body mass index (BMI) thresholds. Generally, candidates must have a BMI of 40 or higher or a BMI of 35 with related health conditions such as type 2 diabetes or heart disease. In some cases, patients with a BMI of 30 or more may qualify if they have type 2 diabetes that is difficult to manage with other treatments.
The procedure can significantly improve or resolve several obesity-related health conditions, making it a viable option for individuals struggling with these medical issues. A multidisciplinary healthcare team conducts a thorough evaluation to ensure the patient’s health status and suitability for the surgery and other weight loss procedures. This evaluation includes physical, psychological, and nutritional assessments to determine the patient’s readiness for the lifestyle changes required post-surgery.
Insurance eligibility is another important factor, as many insurance plans may cover some or all of the surgery costs. Early verification of insurance coverage can help avoid unexpected expenses and ensure a smoother journey toward weight loss goals.
The Surgical Procedure: Step-by-Step
The Roux-en-Y gastric bypass surgery begins with the creation of a small stomach pouch, significantly reducing the amount of food the patient can consume. The first step involves using a surgical stapler to divide the top portion of the stomach from the rest, forming a pouch about the size of an egg. This new stomach pouch limits food intake, helping patients feel full sooner and eat less overall.
Next, the small intestine is rerouted to connect with the newly formed stomach pouch. During this process, the small intestine is divided, and the lower segment is attached to the stomach pouch. This rerouting allows food to bypass most of the stomach and the first part of the small intestine, reducing calorie absorption. Digestive juices from the liver, gall bladder, and pancreas mix with food in the new trunk of the small intestine to enable proper digestion.
The surgical procedure involves the following key points:
- Patients are generally under anesthesia during the procedure.
- The laparoscopic approach allows for smaller incisions and quicker recovery.
- A leak test is performed before concluding the surgery to check the integrity of the connections made.
This meticulous process ensures the surgical procedure is successful and minimizes the risk of complications.
Types of Bariatric Surgeries at Wellstar
Wellstar Comprehensive Bariatric Services offers several types of bariatric surgeries and weight loss surgeries to cater to different patient needs. One of the most common procedures is the Laparoscopic Roux-en-Y Gastric Bypass. This surgery involves creating a small stomach pouch and rerouting part of the small intestine to decrease calorie absorption, leading to significant weight loss.
Another popular option is the Laparoscopic Gastric Sleeve Gastrectomy, which:
- Removes a significant portion of the stomach, resulting in a tube-like structure.
- Limits food intake and helps patients feel full sooner, contributing to effective weight loss.
- Decreases the production of the hunger hormone ghrelin, aiding in appetite control.
For patients requiring more complex solutions, the Biliopancreatic Diversion with Duodenal Switch (BPD/DS) combines a sleeve gastrectomy with a bypass of a substantial section of the small intestine. This procedure is highly effective but comes with a higher risk of complications.
The Modified Duodenal Switch (SADI-S) simplifies the process by connecting only one part of the intestine to the stomach, reducing complication risks while still providing significant weight loss benefits.
Pre-Surgery Preparations
Preparing for gastric bypass surgery involves more than just scheduling the procedure; it requires a comprehensive approach to ensure long-term success. Mental health evaluations are crucial to assess a patient’s readiness for the lifestyle changes required post-surgery. A clear and realistic mindset can significantly impact the overall outcome of the surgery.
Patients should develop a detailed plan regarding nutrition and exercise to support their weight loss journey. Key steps include:
- Meeting with a registered dietitian to learn about necessary dietary modifications before and after surgery.
- Incorporating high-protein, low-calorie meals.
- Avoiding certain foods to help set the stage for a successful recovery.
Establishing a clear plan for preparing for gastric bypass surgery reduces stress and sets patients up for success. This plan should include mental health support, dietary changes, and a structured exercise routine. Addressing these aspects before the surgery date allows patients to approach the procedure with confidence and clarity.
Immediate Post-Surgery Care
The immediate post-surgery period is critical for monitoring complications and ensuring a smooth recovery. Key points include:
- Patients typically stay in the hospital for about two days after the surgery.
- During this time, they are closely monitored for any signs of complications.
- Moderate pain is expected in the first few days.
- Prescribed pain medications are provided to manage discomfort.
Initial dietary guidelines emphasize liquid intake, particularly clear liquids like broth or unsweetened juice. Gradually, patients can introduce more substantial liquids as they tolerate them. This careful progression helps the digestive system adjust to the changes and prevents undue stress on the new stomach pouch.
Patients are usually discharged from the hospital once they can move comfortably and have weaned off pain medications. The transition from hospital to home is a significant step, and following the recommended dietary and activity guidelines is essential for a successful recovery.
Long-Term Recovery and Lifestyle Changes

Long-term recovery from gastric bypass surgery involves a gradual transition from a liquid diet to more solid foods:
- Initially, patients must follow a strict liquid diet to allow the digestive system to heal.
- After about a week, they can consume strained, blended, or mashed foods with a smooth paste consistency.
- Soft foods are typically introduced a few weeks post-surgery.
- Patients can transition to regular foods within six to eight weeks.
Regular physical activity is vital for long-term recovery. Light aerobic exercise, such as walking, is recommended for 30 to 45 minutes per day, three to five times a week as part of an exercise program. This physical activity not only aids in weight loss but also improves overall metabolic health and prevents complications such as sleep apnea and metabolic disorders.
Vitamin and mineral supplements are needed to compensate for changes in nutrient absorption due to the altered digestive system. Daily intake of these mineral supplements is necessary to prevent mineral deficiencies and support overall health. Additionally, hydration is essential, with a recommendation of 1.5 to 2 liters of fluids each day.
Adopting healthy eating habits is vital for maintaining weight loss and losing weight, as well as achieving a healthy weight. Developing a structured meal plan is easier with practical guidance on eating after gastric bypass surgery, which outlines the gradual diet progression and nutrient-rich choices that support sustained weight loss. Key practices include:
- Consuming three to six small meals throughout the day to help manage hunger and maintain energy levels, which can lead to less food intake.
- Stop eating before feeling completely full to avoid discomfort.
- Maintaining dedication to these diet and lifestyle changes.
- Attending regular follow-up consultations to monitor progress and make adjustments.
Importance of Follow-Up Care
Follow-up care is a vital component of the recovery process after gastric bypass surgery. Regular follow-up appointments are essential for monitoring recovery, preventing complications, and ensuring successful weight loss. These appointments allow healthcare providers to evaluate weight loss, manage dietary changes, and address any potential complications that may arise.
Consistent post-surgery monitoring can significantly improve the overall effectiveness of treatment outcomes. It helps in making necessary adjustments to the diet and lifestyle plans, ensuring that patients stay on track with their weight loss goals. Inadequate follow-up can diminish the reliability of data related to the success of bariatric treatments, making it essential for patients to adhere to their follow-up schedules as part of a quality improvement program. In some cases of weight regain or surgical complications, understanding the possibilities and asking can you get gastric bypass twice can help patients evaluate revision procedures and plan for long-term health.
Key aspects of post-surgery care include:
- Regular monitoring of mental health, as patients may experience fluctuations in mood and mental well-being after surgery.
- Attending support groups to enhance weight maintenance and provide a community for sharing challenges and successes.
- Frequent follow-ups and adherence to dietary guidelines to mitigate nutrient deficiency risks and support long-term success.
Emotional and Mental Health Support
Emotional and mental health support is vital before and after gastric bypass surgery to manage emotional changes and aid in adapting to a new lifestyle. Undergoing such a significant procedure can be emotionally challenging, and patients may experience feelings ranging from excitement and hope to anxiety and stress. Having a strong support network can enhance emotional well-being and significantly contribute to long-term success.
Recommended resources for emotional support during gastric bypass surgery preparation include counseling services and support groups. These resources provide a sense of community and shared experiences, which are beneficial for emotional well-being. Support groups can offer practical advice, encouragement, and a platform to discuss challenges and successes with others who have undergone similar experiences. Maintaining emotional balance is critical, and the strategies shared in the importance of psychological support before and after gastric bypass surgery highlight how counseling and support groups can strengthen mental well-being and improve surgical outcomes.
Developing healthy sleep and stress management habits is also encouraged before undergoing surgery. Good sleep and stress management improve overall health and support the body’s ability to cope with the changes brought about by the surgery. Engaging with a healthcare team that includes mental health professionals ensures that patients receive comprehensive care that addresses both physical and emotional needs.
Achieving Lasting Weight Loss and Better Health
Gastric bypass surgery offers a powerful, long-term solution for individuals struggling with severe obesity and related health conditions. By reducing stomach size and rerouting digestion, this procedure supports significant weight loss, improved metabolic health, and the reduction of chronic issues such as diabetes and hypertension. Success relies on careful preparation, consistent follow-up care, and a lifelong commitment to healthy habits.
At Wellstar Comprehensive Bariatric Services, we provide expert guidance and personalized care for those considering gastric bypass surgery in Marietta, Cobb County, Smyrna, LaGrange, West GA, and Austell. Our dedicated team will support you through every step, from initial evaluation to recovery and long-term wellness, helping you achieve sustainable results and a healthier, more active life.
Frequently Asked Questions
Who is eligible for gastric bypass surgery?
Candidates generally need a Body Mass Index (BMI) of 40 or higher, or a BMI of 35 with related health issues such as type 2 diabetes or hypertension. A thorough medical, nutritional, and psychological evaluation ensures readiness for the required lifestyle changes and long-term success.
How much weight can I expect to lose after gastric bypass surgery?
Most patients lose about 60–80% of their excess body weight within 18 to 24 months. Results vary depending on adherence to post-surgery dietary guidelines, exercise routines, and follow-up appointments with healthcare providers.
What is the recovery time after gastric bypass surgery?
Recovery typically takes four to six weeks. Patients often stay in the hospital for one to two days and progress from a liquid diet to soft foods, then regular foods, over several weeks. Light exercise is encouraged early to aid healing and prevent complications.
Will I need to take vitamins and supplements after surgery?
Yes. Because the digestive system absorbs fewer nutrients after surgery, lifelong vitamin and mineral supplementation—such as multivitamins, calcium, vitamin B12, and iron—is essential to avoid deficiencies and maintain overall health.
How important is follow-up care after the procedure?
Follow-up care is crucial for monitoring weight loss progress, adjusting nutrition plans, and identifying any complications early. Regular visits with your bariatric team and participation in support groups help reinforce lifestyle changes and ensure long-term success.
